Considering Stem Cell Therapy? Here’s What You Need to Know Before Visiting a Clinic in Cancun or Tijuana
- Misael González

- Jul 30, 2025
- 35 min read

Interest in stem cell therapy has surged in recent years, with medical tourists often looking to places like Cancun or Tijuana for treatment. A Cancun stem cell clinic or Tijuana stem cell clinic may promise relief for joint pain, injuries, or chronic conditions at a lower cost than U.S. clinics. But before you sign up for stem cell therapy in Cancun, it’s crucial to understand the science, the process, and how to choose a reputable provider. In this article, we focus on mesenchymal stem cells (MSCs) – the most commonly used cells in these therapies – and provide an evidence-based overview for patients seriously evaluating MSC treatment (often called MSC therapy Tijuana or Cancun). We’ll cover what MSCs are, what conditions they treat (from osteoarthritis to autoimmune disease), how they compare to platelet-rich plasma (PRP), what a typical session involves (including cost ranges in Mexico), how to spot a legitimate clinic, and more. The goal is a realistic, hype-free guide so you can decide if traveling for stem cell therapy is right for you.
Foundational Explanation: What Are Mesenchymal Stem Cells (MSCs)?

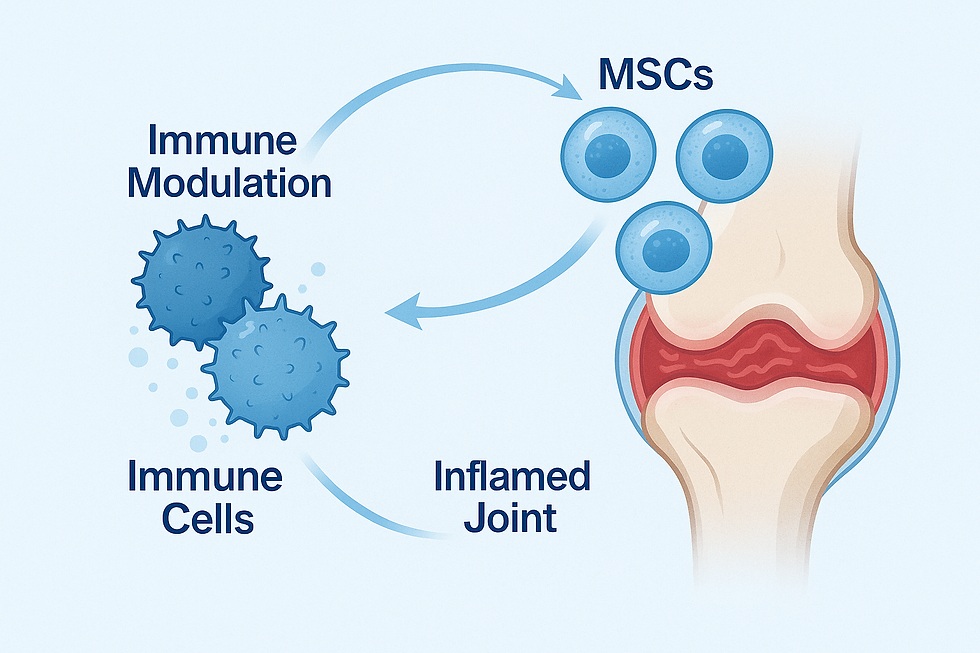
Mesenchymal stem cells (MSCs) are a type of adult stem cell found in many tissues of the body. They are multipotent, meaning they can differentiate into a variety of tissue types – classically bone, cartilage, and fat cells . MSCs also have powerful effects on healing: they secrete anti-inflammatory and growth factors that help repair damage and modulate the immune system . In the body, MSCs act like the “repairmen” – they migrate to injured or inflamed areas and release signals to promote tissue regeneration and reduce inflammation.
Sources of MSCs: MSCs can be harvested from several sources. The most common sources are: bone marrow (typically from the hip bone), adipose tissue (fat, often from a mini liposuction), and birth tissues like the umbilical cord or placenta. You might encounter terms like autologous MSC therapy Mexico, which means using your own stem cells (harvested from your body, processed, and re-injected). Alternatively, some clinics offer donor-derived cells – for example, placental MSC treatment in Cancun refers to using MSCs collected from donated placenta or umbilical cord tissue. The treatments are regulated as either autologous (self-to-self) or allogeneic (donor cells) – both approaches are used in Mexico . Autologous MSC therapy has the advantage of using your own cells (eliminating immune rejection issues), while donor (allogeneic) MSCs from sources like placenta can be prepared in advance and don’t require you to undergo a cell harvest procedure.
How MSC therapy works: Unlike a drug that targets a single pathway, MSCs work in multifaceted ways. They can turn into the specific cell types needed to rebuild cartilage or other tissues under the right conditions . More importantly, they act as “medicinal signaling cells” – releasing cytokines, growth factors, and exosomes that reduce inflammation and guide the healing process . For example, MSCs secrete molecules like TGF-β and IL-10 that dampen an overactive immune response and encourage repair . This immunomodulatory ability is why MSCs are being used not only for orthopedic issues but also for autoimmune diseases and even chronic inflammatory conditions. In summary, MSC therapy aims to boost the body’s natural healing: by injecting a concentrated dose of these repair cells, we hope to accelerate tissue regeneration and calm harmful inflammation.
Conditions Treated With MSCs
Clinics in Cancun and Tijuana advertise MSC therapy for a wide range of conditions. Here we focus on several high-demand uses: osteoarthritis, sports injuries, autoimmune diseases (like rheumatoid arthritis), neurological disorders, and chronic pain. For each, we’ll discuss how MSCs might help, expected improvements, scientific evidence (especially from 2023–2025 studies), and how long it may take to see results.
Osteoarthritis (Joint Degeneration)

Osteoarthritis (OA) – particularly knee osteoarthritis – is one of the most common reasons patients seek MSC therapy. In fact, if you search online for stem cell osteoarthritis Cancun, you’ll find many clinics offering MSCs joint pain treatment in Cancun for worn-out knees and hips. The rationale is that MSCs can potentially regenerate cartilage and reduce joint inflammation. When injected into an arthritic joint, MSCs may differentiate into chondrocytes (cartilage cells) and produce extracellular matrix, helping repair cartilage lesions . Even more immediately, they secrete anti-inflammatory factors to soothe the inflamed joint lining (synovium), which can reduce pain and swelling.
Expected improvements: Patients with knee OA who receive MSC injections often report reduced pain and improved function in the months following therapy. High-quality evidence backs this up: a 2025 systematic review of randomized trials (8 RCTs, 502 patients) found that an MSC knee injection led to significant pain relief and functional improvement at 6 months and 12 months compared to placebo . Specifically, treated patients scored better on the WOMAC arthritis index (with improvements that continued a year out), and importantly there was no increase in adverse events versus control . In practical terms, this means MSC therapy helped patients walk farther, climb stairs more easily, and experience less daily joint pain than those who didn’t get the stem cells. Another analysis noted that using higher doses of MSCs (or MSCs derived from adipose tissue) was associated with better outcomes . While results vary, clinical trials generally show moderate improvements in pain and function – not a complete cure or cartilage regrowth to that of a young joint, but often enough improvement to delay surgery like knee replacement .
Timeframe for results: MSC therapy is not an overnight fix; it triggers a gradual healing process. Most studies and patient reports indicate that benefits appear gradually over a period of 1–3 months, with further gains at 6 months and even 12 months post-injection . For example, pain might start diminishing a few weeks after the injection as inflammation subsides, but measurable improvements in joint function often peak around the 3- to 6-month mark as tissue repair takes place. Patients should maintain realistic expectations – you may not feel much change in the first few weeks, but over a few months you could notice you’re taking fewer painkillers and moving easier. Combining the therapy with physiotherapy and exercise can further enhance results.
Sports Injuries (Tendons, Ligaments, Cartilage)

Athletes and active individuals are drawn to stem cell therapy to recover from sports injuries like tendon tears, ligament sprains, or cartilage damage. MSCs have been used for difficult-to-heal tissues such as the Achilles tendon, rotator cuff in the shoulder, or meniscus in the knee. The idea is to harness the regenerative power of MSCs to speed up repair of tendons and other musculoskeletal tissues that normally heal slowly. For instance, in a tendon injury, injected MSCs can become tendon cells (tenocytes) and produce new collagen fibers, while also releasing growth factors that attract blood flow and healing cells to the area .
Expected improvements: The evidence, while still emerging, is encouraging. A 2021 meta-analysis looked at MSC therapy for chronic tendon disorders (including conditions like tennis elbow and rotator cuff tears). It found that MSC-treated patients had significantly less pain and better functional scores than before treatment – in fact, the pooled effect size for pain relief was quite large . Improvements were not only subjective (pain relief) but also visible: follow-up MRIs and ultrasounds showed healthier tendon tissue in many cases . This suggests the MSCs were actually contributing to tissue repair, not just masking pain. Athletes who receive MSC injections for, say, a partial ACL tear or chronic tendonitis often report faster return to activity and more complete healing than with standard rest and therapy alone. It’s important to note many of these studies were small or observational, but the trend is that MSC therapy can enhance recovery from sports injuries, especially for injuries that haven’t responded to conventional treatments.
One notable finding is a dose-dependent response – higher cell doses led to greater pain relief in tendon injuries . This implies that for severe injuries, a robust dose of MSCs might be needed to see a substantial benefit. Also, many sports medicine specialists combine MSCs with platelet-rich plasma (PRP) or other adjuncts to maximize healing (we discuss PRP vs MSC in the next section). Overall, if you have a stubborn tendon or ligament injury, MSC therapy could potentially help you heal and get back to sports sooner, though it should complement, not replace, proper rehab exercises.
Timeframe: Recovery timelines vary with the injury, but generally expect a few months to see full benefits. In tendon healing, studies with MSCs showed improvements in pain and function around 3–6 months post-treatment . For example, an athlete with a chronic tennis elbow might start noticing reduced pain and better grip strength within 1–2 months, with tendon imaging showing repair by 6 months. Patience is key; you’ll still need to rest and rehabilitate the injury – the stem cells simply accelerate the natural healing cascade.
Autoimmune Diseases (e.g. Rheumatoid Arthritis)
Beyond orthopedic uses, MSC therapy is being explored for autoimmune diseases like rheumatoid arthritis (RA), lupus, and others. Autoimmune conditions are characterized by an overactive immune system attacking the body’s own tissues. MSCs, with their immune-regulating abilities, offer a novel approach: they can calm down immune cells and reduce inflammatory attacks on joints and organs . In RA, for example, MSC infusions (usually given intravenously rather than into a joint) aim to reduce joint inflammation, prevent further joint damage, and induce remission alongside conventional medications.
Expected improvements and evidence: Early clinical trials and reviews suggest MSC therapy can reduce disease activity in rheumatoid arthritis. A recent 2025 meta-analysis of 42 trials involving various autoimmune and rheumatic diseases (including RA) concluded that MSC treatment showed promise in improving symptoms of RA and other conditions, with a favorable safety profile . Patients in small RA studies have experienced reductions in swollen joint counts and inflammatory markers after MSC therapy . For instance, one trial reported that RA patients given MSC infusions had fewer painful joints and lowered systemic inflammation compared to baseline, hinting at a “reset” of the immune system. It’s not a mainstream RA treatment yet, but these proof-of-concept studies show that MSCs can dial down the autoimmune response and potentially induce remission in some cases.
It’s worth noting that results can be variable – some RA patients respond markedly, while others see only mild changes. Autoimmune diseases are complex, and MSC therapy is still considered experimental in this realm. However, importantly, safety has been reassuring: MSC-treated autoimmune patients did not experience more adverse effects than controls in aggregated studies . No life-threatening side effects have emerged, and unlike immunosuppressive drugs, MSCs do not seem to broadly weaken the immune system (they modulate it rather than shut it down).
Beyond RA, MSCs are under investigation for lupus, multiple sclerosis (MS), inflammatory bowel disease, and more . In lupus (SLE), a meta-analysis noted significant improvement in disease activity scores after MSC therapy . For MS (an autoimmune neurological disease), the results have been mixed – the 2025 review found that MSCs did not significantly improve disability in established multiple sclerosis , though research is ongoing. Neurological autoimmune conditions may need different strategies or higher doses. Overall, if you have an autoimmune condition that is not well controlled by standard treatments, MSC therapy (available in places like Mexico as an advanced treatment) might be an option to discuss with your doctors. It’s not a cure, but some patients have seen their disease go into a quieter state for some time after MSC infusions.
Timeframe: In autoimmune cases, MSC therapy might show benefits within weeks to a couple of months. For example, RA patients in some studies saw improvements in symptoms by 1–3 months post-infusion. The effect may last 6–12 months or more, but repeat treatments could be needed to maintain remission (this is an active area of study). It’s also common that MSC therapy is used alongside conventional drugs, not necessarily as a standalone replacement – at least until more evidence accumulates.
Neurological Disorders

MSC therapy is even being tested for certain neurological disorders – ranging from stroke and spinal cord injury to neurodegenerative diseases like Parkinson’s. The idea might sound far-fetched, but it ties back to MSCs’ abilities to reduce inflammation and secrete growth factors that support neural tissue. For instance, after a stroke, there is inflammation and cell death in the brain; an IV infusion of MSCs can home to the damaged brain tissue and release factors that promote new blood vessel growth and neural repair. In conditions like Parkinson’s or motor neuron disease, MSCs might help by providing neurotrophic (nerve-growing) factors or modulating the immune aspects of those diseases.
Evidence and expected outcomes: Among neurological applications, stroke recovery has some of the strongest data. A 2024 meta-analysis in Stem Cells Translational Medicine reviewed 15 RCTs in ischemic stroke patients and found that MSC-treated patients had better recovery outcomes than those without MSCs . Specifically, patients who received MSCs showed greater improvements in their ability to perform daily activities (as measured by the modified Rankin Scale) and had better neurological function scores . Impressively, the stem cell treated group also had a lower mortality rate after stroke – in the analysis, the risk of death was less than half that of controls (RR ~0.44) . This suggests MSC therapy may aid in tissue recovery to the point of improving survival in acute stroke. Adverse effects in these stroke trials were minor (common ones included transient fever or headache) , indicating it’s a safe add-on therapy. While stroke patients aren’t magically cured, MSC therapy can mean the difference between being wheelchair-bound and regaining the ability to walk with minimal assistance in some cases, as anecdotal reports have shown.
For spinal cord injury (SCI), a few trials have injected MSCs (sometimes intrathecally into the spinal fluid) in patients with paralysis. There are individual cases of improved sensation or motor function, and one trial reported reduced neuropathic pain and improved quality of life in MSC-treated SCI patients . However, outcomes vary widely depending on injury severity and time since injury.
In degenerative neurological diseases like Parkinson’s or Alzheimer’s, research is still in early phases. Some small studies in Parkinson’s disease hinted at motor symptom improvements, but it’s too early to know how effective MSCs will be. Multiple sclerosis (MS), which we mentioned earlier, is a hybrid case – it’s autoimmune but affects the nervous system. Trials of MSCs in MS have shown the therapy is safe and can transiently reduce immune activity; however, consistent clinical improvements (like better walking ability or fewer relapses) have been hard to prove, and one meta-review did not find significant functional benefits in MS patients so far . This doesn’t close the door on MSCs for MS – it just means more research is needed and perhaps repeated dosing or different delivery methods (like via spinal fluid) might be required to see an effect.
Timeframe: Neurological healing tends to be slow. In stroke or acute injuries, MSCs are often given within weeks to months of the event, and improvements may unfold over the next 3 to 6 months as the brain or spinal cord rewires and heals . For chronic neurodegenerative conditions, if improvements occur, they might be subtle and take a few months to observe (for example, a Parkinson’s patient might notice slight improvement in tremor or slowness over 2–4 months). It’s important to maintain therapy like physical rehabilitation – MSCs are a boost, not a standalone fix.
Chronic Pain

“Chronic pain” is a broad category, but here we refer to conditions like chronic back pain (degenerative disc disease), joint pain that isn’t just simple arthritis, or even complex regional pain syndrome. The rationale for using MSCs in chronic pain conditions is usually either to address an underlying degeneration (e.g., regenerate a degenerated spinal disc or facet joint) or to reset aberrant inflammation or nerve pain signals. For example, in chronic low back pain due to a worn-out intervertebral disc, doctors have injected MSCs into the disc space in hopes of restoring disc cartilage and reducing pain.
Expected improvements: There is some early clinical evidence that MSC therapy can help certain chronic pain sufferers. In degenerative disc disease, a randomized trial of allogeneic MSC injections into painful discs showed patients had significant pain reduction and improved function at one year compared to placebo in some studies (though not all studies are uniformly positive). A phase I trial in 2023 reported that MSC injections for chronic back and neck pain were safe and yielded pain relief in most patients, without serious complications . Patients often report gradual decreases in pain scores and an increased ability to perform daily activities they had avoided. For conditions like neuropathic pain, MSCs have been tested in small studies (for example, in refractory peripheral neuropathy or post-spinal cord injury pain) with hints that they can alleviate pain intensity and improve quality of life . The MSCs may be reducing inflammation around nerves or even supporting nerve repair, thereby lessening pain signals.
It’s important to stress that chronic pain can have many causes, and MSCs are not guaranteed to help every type of pain. If pain is due to extensive scar tissue or central nervous system changes, stem cells might have limited effect. But if there’s an ongoing tissue injury or inflammation component, MSCs could provide relief by healing that tissue. Patients considering MSC therapy for chronic pain should have a thorough evaluation to pinpoint the pain source and ensure that a regenerative approach makes sense for their case.
Timeframe: As with other uses, don’t expect instant pain relief in chronic conditions. Many patients see incremental improvement over a few months. For instance, someone with chronic knee pain who gets an MSC injection might notice slight pain reduction at 1 month, moderate improvement by 3 months, and maximum benefit by 6 months. The pain relief can sometimes last a long time (6 months to a couple of years in some reports), potentially delaying the need for surgeries or higher-risk interventions. Keep in mind that some patients may require a series of treatments – e.g., two or three MSC injections spaced out over 6-12 months – to optimize pain control, especially if the condition is severe.
PRP vs. MSC vs. Both: What’s the Difference?

You might have also heard of platelet-rich plasma (PRP) therapy, which is commonly used for sports injuries and arthritis. How does PRP compare to MSC therapy, and do you need both? This section will clarify the differences and when each option (or a combination) is appropriate.
Platelet-rich plasma (PRP) is not a stem cell treatment; it’s a concentration of platelets derived from your own blood. A small sample of your blood is spun in a centrifuge to separate out the platelet-rich layer, which is then injected into the injury site. Platelets release growth factors that can stimulate healing of tissue. PRP is popular for treating mild to moderate osteoarthritis, tendonitis, and muscle strains. It reduces pain and inflammation and can jump-start a healing response, but PRP does not create new tissue – it’s more about signaling the body to repair itself. PRP is relatively easy and inexpensive (compared to stem cells) and typically done in 1 to 3 injection sessions.
Mesenchymal stem cells (MSCs), as discussed, are living cells that can both secrete healing factors and potentially turn into new tissue cells. Obtaining MSCs is more involved than drawing blood for PRP; it may require a bone marrow aspiration or a mini liposuction to collect cells (unless donor MSCs are used). MSC therapy is often chosen for more severe conditions – for example, advanced osteoarthritis or complex injuries – where mere growth factors from PRP might not be sufficient. MSCs not only reduce inflammation but also actively regenerate tissue to an extent. They are also being used for systemic conditions (like autoimmune disease) where PRP has no role. The downside is cost and complexity: MSC treatments cost more and must be done in a properly equipped facility.
Combined MSC + PRP therapy: Some clinics (especially in Mexico) offer to do both – inject MSCs along with PRP, or one after the other. You might see this marketed as MSC PRP therapy Cancun or a similar term. The rationale is that PRP can provide a nutrient-rich environment that helps the injected MSCs thrive and work better, somewhat like “fertilizer” for the stem cells. In joint treatments, a doctor might inject MSCs into the knee and then also inject PRP (either mixed together or sequentially) to maximize the regenerative stimulus.
But is combining them more effective? The science is still evolving. Interestingly, a comprehensive review of knee osteoarthritis treatments found that MSCs alone had a superior effect on outcomes compared to PRP alone, and that combining PRP with MSCs offered no significant advantage over MSCs by themselves in terms of pain and function improvement . In other words, MSCs seem to do the heavy lifting; adding PRP didn’t markedly change the results, at least in that analysis. That said, PRP is relatively harmless to add and may yet have synergistic benefits (some theories suggest PRP helps recruit the MSCs to the right place and keeps them active). Clinically, some practitioners swear by combining them for tough cases, while others reserve combination therapy for specific scenarios.
To summarize these differences, here is a simple comparison:
Therapy | Description | Best For |
PRP (Platelet-Rich Plasma) | Injection of concentrated platelets from your own blood. Platelets release growth factors that stimulate tissue repair and reduce inflammation. Contains no stem cells. | Mild-to-moderate injuries or early osteoarthritis, tendon or ligament sprains, and muscle tears. PRP is often a first-line regenerative therapy for joint pain or sports injuries when damage is not severe. It’s lower cost and low risk, but primarily provides a short-term boost to healing. |
MSCs (Mesenchymal Stem Cells) | Injection of stem cells (either autologous or allogeneic) that can differentiate into cartilage, bone, etc., and secrete anti-inflammatory and regenerative factors. Typically requires harvesting cells (from bone marrow, fat, or donor tissue) and processing them in a lab before injection. | More advanced degeneration (e.g. moderate to severe osteoarthritis – cases often marketed as MSC joint pain treatment), persistent injuries that haven’t healed with standard care, and systemic conditions (autoimmune, etc.). MSC therapy is chosen when tissue damage or inflammation is significant and we need a stronger, longer-lasting regenerative effect. |
Combined MSC + PRP | A combination approach where PRP is used alongside MSCs, either mixed together or given sequentially. The PRP may help create a supportive environment for the stem cells. | Situations where maximal healing is desired – for example, a difficult knee osteoarthritis case or a major rotator cuff tear. Some Cancun clinics offer MSC PRP therapy as a premium service. Evidence is still limited on added benefit; one study noted that adding PRP to an MSC knee treatment did not significantly improve outcomes beyond MSCs alone . However, combined therapy might make sense in theory for individual cases, and research is ongoing. |
Which to choose? In general, if your condition is mild and primarily needs a nudge to heal, try PRP first (since it’s simpler and cheaper). If your condition is more severe or has a degenerative component (like bone-on-bone arthritis or a major tendon tear), MSCs are more potent and appropriate. You might also do PRP first and, if it’s not sufficient, move to MSCs. Many clinics will recommend a treatment plan tailored to your specific case – for example, an athlete with a partial ligament tear might get a PRP injection initially; if healing stalls, an MSC injection might be the next step. For systemic diseases (like rheumatoid arthritis or multiple sclerosis), PRP is not used (since it won’t affect an autoimmune process) – MSCs or other cell therapies are the focus there.
If you decide on MSC therapy, don’t be afraid to ask the clinic if they use PRP as well or why/why not. A transparent provider will explain their rationale. Some do include PRP by default with MSCs (as a combo package) whereas others do not.
What to Expect From a Stem Cell Session (in Cancun or Tijuana)

If you’re planning to visit a clinic in Cancun or Tijuana for MSC therapy, it helps to know what the process will look like. While details vary by clinic, a typical MSC treatment session in Mexico involves the following steps:
· Consultation and Evaluation: First, you’ll have a detailed consultation with the clinic’s physician (this can sometimes happen remotely by video call before you travel). They will review your medical history, current condition, and any imaging (X-rays, MRIs) to confirm you’re a candidate for MSC therapy. They’ll discuss whether they will use your own cells or donor cells. For example, if you’re undergoing autologous MSC therapy in Mexico, they might schedule you for a cell harvesting procedure; if using donor (placental MSCs or umbilical cord cells), they will have those prepared from a lab.
· Preparation: On the day of treatment, if using autologous cells, the medical team will collect them. For bone marrow MSCs, this means a bone marrow aspiration – typically under local anesthesia (and sometimes mild sedation) a doctor uses a needle to draw marrow from the back of your hip bone. It’s a short procedure (15-20 minutes) and feels like pressure in the hip; local anesthetic makes it tolerable, though some soreness can follow. If using adipose (fat)-derived MSCs, they’ll perform a mini liposuction (often from the abdomen or flank) under local anesthesia to suck out a small amount of fat. Both methods are outpatient procedures. If using donor cells (placental/umbilical), obviously you skip this harvesting step – the clinic will request vials of frozen MSCs ready from a lab.
· Processing: After harvesting, if autologous, the sample (bone marrow or fat) is taken to a laboratory on-site or nearby. There, technicians isolate the MSCs. In some clinics, they may culture-expand the cells to get a higher count (Mexico permits cell expansion in certified labs, unlike the U.S. ). This processing can take a few hours to a day. In many same-day protocols, they will do a minimal processing: spin down the bone marrow to concentrate the cells (producing something called bone marrow concentrate which is rich in MSCs and growth factors) and use it within hours. In other cases, if they expand cells, you might come back another day for the injection after the cells have multiplied. Make sure to ask your clinic about their process – reputable clinics use GMP-compliant labs to ensure cell product quality.
· Administration (Injection or Infusion): The actual delivery of the MSCs depends on your condition. For orthopedic problems, injections are common – e.g. injecting into the knee joint, hip joint, or around a tendon. The area will be numbed with local anesthetic, and often ultrasound or x-ray guidance is used to precisely place the cells at the injury site. If it’s a spine issue or disc, they may use fluoroscopy (real-time X-ray). For systemic or more diffuse conditions (like autoimmune or neurological issues), the MSCs might be given intravenously (IV) into a vein, so the cells can travel through your bloodstream to areas of inflammation. Some protocols for neurological conditions even inject cells into the spinal fluid (intrathecal injection) to access the brain/spinal cord – though this is more specialized. The procedure itself is usually quick, maybe 30 minutes for an IV or a few minutes for a joint injection. Sedation is generally not needed except for bone marrow harvest or if someone is particularly anxious.
· Post-treatment and Recovery: MSC therapy is typically an outpatient procedure – you won’t be hospitalized. After the injection/infusion, you’ll be observed for a short time (maybe an hour) to ensure there are no immediate reactions (which are rare). Most people feel fine to walk out and resume light activities later that day. If you had a bone marrow draw, your hip might be sore for a couple days – expect some bruising and tenderness there, managed with mild painkillers. Joint injections can cause temporary flare-up of pain or swelling for 1–2 days due to the injection itself; icing the area and rest can help. The clinic will give you specific after-care instructions, which often include avoiding strenuous activity for a week or two. For example, if you got a knee injection, you might be asked to use a cane or minimize weight-bearing for a couple of days and avoid high-impact exercise for a few weeks to allow the cells to do their work without excess stress on the joint.
· Follow-up: Many clinics schedule a follow-up evaluation the next day (especially if you traveled internationally, they want to check on you before you fly home). After that, follow-ups might be via phone or video call at 1 month, 3 months, 6 months, etc. Some clinics will request that you send progress reports or even repeat imaging to gauge improvement. It’s a good idea to keep a symptom diary so you can report how your pain or function changes over time. Depending on results, some patients plan a return visit for another session if needed (some conditions might benefit from 2-3 rounds of MSC therapy over a year for maximum effect).
· Downtime: One of the selling points of stem cell therapy is the minimal downtime. There is no large incision or major anesthesia (unless a mini lipo is considered, but that’s minor). Most patients are up and about the same or next day. If you traveled to Cancun, you could theoretically have the injection on one day and be relaxing on the beach the next (just avoid extreme activities). Flying back home is usually allowed within a day or two after treatment, but always confirm with the medical team – occasionally they might want you to stick around for 2-3 days if any lab processing or follow-up checks are needed.
· Results timeline and rehabilitation: As covered earlier, improvements come gradually. The clinic should give you realistic guidance that you shouldn’t expect immediate miracles. They will likely encourage you to maintain a healthy lifestyle, possibly physical therapy or specific exercises, and to be patient as the healing process unfolds over weeks to months.
Typical pricing in Cancun/Tijuana: The cost for MSC therapy in Mexico is significantly lower than in the United States, but it’s still a substantial investment. Prices can vary depending on the number of cells, source of cells, and reputation of the clinic. On average, expect to pay around US $3,000–$6,000 per treatment session in Cancun. For example, some clinics advertise packages like anti-aging MSC treatments in Cancun for about $3k–$6k . Treatments for more complex diseases or higher cell doses (or multiple joints) could cost more – sometimes $8,000–$10,000 or higher, especially if multiple sessions are bundled. In Tijuana, prices are often similar, though one report noted Cancun can be a bit cheaper on average . Always clarify what the quoted price includes: Does it cover the cell harvesting and lab processing? (Usually yes.) Does it include complementary therapies like PRP or exosomes? Does it cover follow-up or just the initial injection? Also, factor in travel costs – although even with airfare and hotel, many patients still save money compared to a single $20k+ stem cell infusion in the U.S.
Most clinics require payment upfront and are cash-based (insurance generally does not cover experimental stem cell treatments). Be wary of any clinic that is dramatically cheaper than others – if someone offers a $1,000 stem cell therapy that normally costs $5,000, that’s a red flag. It costs money to properly source and handle cells; a cut-rate price could indicate corners are being cut (like low cell counts or subpar lab practices). On the flip side, the most expensive clinic isn’t necessarily the best – look for transparency and value. A legitimate clinic will be clear about pricing and exactly what you get for the cost.
What Makes a Clinic Legitimate? (Checklist for Safety)
Stem cell therapy is a cutting-edge field, and unfortunately not all providers follow best practices. If you’re considering a Cancun stem cell clinic or Tijuana stem cell clinic, do your homework to ensure the clinic is legitimate, safe, and compliant with regulations. Here’s a checklist of things to look for:
· COFEPRIS Licensing: COFEPRIS (the Mexican health regulatory agency, analogous to the FDA) strictly oversees regenerative medicine clinics. A reputable clinic must have specific licenses from COFEPRIS to legally provide stem cell treatments. Ask the clinic to provide proof of their licenses. Important ones include: a Regenerative Medicine license (which authorizes the clinic to administer cell therapies) and, if they handle cells on-site, a Cell Bank license (for processing/cryopreserving cells) and a Collection license (if harvesting tissues like bone marrow or fat) . Medical offices without a regenerative medicine license cannot legally infuse stem cells in Mexico – COFEPRIS requires verification of proper equipment, trained personnel, and emergency procedures before granting this . Legitimate clinics will often display their COFEPRIS registration or license number on their website or clinic wall. You can even contact COFEPRIS to double-check a clinic’s status if you’re uncertain. The licensing process is rigorous (it can take months and many inspections) , so having those credentials is a good sign that the clinic meets basic safety standards.
· GMP-Certified Lab and Quality Control: Find out where the stem cells are processed. High-quality clinics either have an in-house laboratory that meets GMP (Good Manufacturing Practice) standards or partner with a certified cell bank. GMP standards ensure that the cells are prepared in sterile conditions, are properly tested for contamination, and are viable and potent for use. For example, some Mexican clinics indicate they use cGMP- and ISO-certified laboratories for their cell products. This level of quality control is what you want – it means the lab follows international standards similar to those a pharmaceutical factory would follow. Avoid clinics that can’t clearly explain how/where the cells are processed or that refuse to disclose their cell source. Also, if donor cells are used, ensure they come from an authorized tissue bank with ethical sourcing and thorough donor screening (for infectious diseases, etc.). The clinic should be able to provide documentation or at least a clear description of their cell source (e.g., “we use umbilical cord MSCs provided by XYZ Biobank which is licensed by COFEPRIS”).
· Qualified Medical Staff: Look into the credentials of the doctors and staff. The treatments should be provided by a licensed physician (MD or equivalent) with relevant training (professional certificate in medicine) – often this might be an orthopedic surgeon, sports medicine specialist, pain management specialist, or even immunologist, depending on what is being treated. Check if the doctor has experience in the field of regenerative medicine or any certification in it. You want someone who can handle complications if they arise. Additionally, a good clinic will have a multidisciplinary team – for example, radiologists or ultrasound experts to guide injections, nurses biotechnology, microbiology, to assist and monitor patients, and proper handling of stem cells and/or biologics. Physician credentials can be verified: in Mexico, doctors have a cedula (license number). You can ask for this number and look it up in public databases to ensure they are legitimate. A red flag is if a clinic is run by someone who is not a medical doctor or if no specific doctor’s name is associated with the treatments.
· Transparent Protocols and Patient Evaluation: A reputable clinic will evaluate you carefully and only treat you if you’re a suitable candidate. They should not promise to treat every condition under the sun without evidence. Be cautious if a clinic’s website claims 100% success rates or says “we can cure Parkinson’s, diabetes, autism, spinal cord injury, and more” all in one place without citing any data – that’s usually a sign of hyperbole. Legit clinics tend to specialize or at least give realistic ranges of what they treat (and what they don’t). They should also inform you of potential risks and the experimental nature of some uses. During the consult, notice if they encourage you to ask questions and if they answer them clearly. The clinic should also obtain informed consent, having you sign documents that outline the procedure and its risks/benefits. If they try to have you sign a waiver without discussion, or if you feel like you’re getting a sales pitch more than a medical consultation, reconsider.
· Checklist for Safety Features: Here are a few quick things to verify:
o The clinic’s address and license names match. Scammers might show a license that actually belongs to a different address or company; ensure the paperwork corresponds to the actual clinic location .
o They have an emergency plan and necessary equipment. In the rare event of a severe allergic reaction or complication, do they have medications and trained staff to handle it on-site? (COFEPRIS checks for this in licensing).
o Follow-up care: Will the clinic be available to you after you go home if you have questions or issues? Good clinics stay in touch and may coordinate with your home physician.
o No outrageous claims: If a clinic uses words like “miracle cure” or guarantees results, that’s unethical. Science-based providers will be optimistic yet honest that results vary and not everyone responds.
o Patient testimonials/case studies: While these are not scientific evidence, seeing some real patient stories (especially if they can connect you with a past patient to talk to) can provide insight. Legit clinics often have patients who are willing to share their experience (with permission).
o Regulatory environment: Know that Mexico does have regulations – COFEPRIS has shut down clinics operating illegally in the past. So if a clinic is operating, it doesn’t automatically mean it’s licensed. Do your due diligence on their regulatory status.
In short, a little healthy skepticism goes a long way. Many clinics in Cancun and Tijuana are doing fantastic, cutting-edge work within the bounds of the law and ethics – but a few “bad apples” exist. Use the above points to vet your options. When you find a clinic that checks all the boxes, you can feel more confident proceeding, knowing your safety and the quality of treatment are being prioritized.
Real Patient Scenario: MSC Therapy in Action

To illustrate what MSC therapy can achieve (and what it’s like), let’s look at a realistic patient scenario. Keep in mind individual results vary, but this scenario is based on reported outcomes and typical cases:
Meet John, a 55-year-old from Texas with knee osteoarthritis. John has moderate-to-severe arthritis in his left knee – years of running and an old sports injury have worn down his cartilage. He’s in daily pain, walks with a limp, and had been told he might need a knee replacement in a few years. Wanting to avoid surgery, John researched alternatives and found a Cancun stem cell clinic that offers MSC treatments for joint pain. After consulting with the doctors, he decided to try an MSC joint pain treatment in Cancun.
John’s treatment involved an autologous MSC therapy approach. On day one, the clinic’s orthopedic specialist harvested 50 mL of bone marrow from John’s pelvic bone. The discomfort was minimal – he was awake and just felt pressure (they used local anesthetic and mild IV sedation). That marrow was processed the same day in their lab to concentrate the MSCs. In the afternoon, John received an injection of his concentrated MSCs directly into his knee joint (guided by ultrasound). The procedure was quick; the knee was numbed, and he said it felt like a regular steroid injection he once had, just with a bit more fluid going in causing fullness feeling.
After the injection, John rested in his hotel for the next two days (the clinic advised him to take it easy, wear a knee brace, and ice intermittently). He noticed his knee was a bit swollen for the first 48 hours – which he was told might happen due to the injection – but he managed with Tylenol and ice. Importantly, no major side effects or complications occurred. He flew back home on day three.
The results: For the first month, John didn’t notice much change and admittedly felt a bit worried. But by around 6 weeks, he realized he wasn’t reaching for pain meds as often. He could get through a morning walk with less stiffness. By the 3-month mark, John’s improvement was in full swing – he reported his knee pain went down by about 50%, and his walking endurance doubled. He could climb stairs again without significant pain, something he hadn’t done in a year. At a 6-month follow-up, John’s orthopedic doctor back home was impressed: John’s knee had better range of motion and he scored much lower on his WOMAC arthritis disability score (a reflection of less pain and better function). This aligns with clinical studies, which have found around 50–60% improvement in knee arthritis symptoms at 6–12 months after MSC therapy .
John’s quality of life greatly improved – he was able to resume light jogging and cycling. It wasn’t a complete cure: he still had some achy days and knew his knee was not “brand new.” However, the progression of arthritis seemed to have stalled and even slightly reversed in terms of pain and function. Two years later, John still hasn’t needed that knee replacement, and he’s considering going back for a second MSC booster injection to strengthen the gains (some clinics recommend a follow-up treatment after 1–2 years if needed).
Why John’s story is important: It shows a plausible outcome – significant improvement but not magic. Patients reading this should understand that while some people are “super responders” (with dramatic improvements), others may get modest benefits or sometimes not much change at all. John’s case also highlights the typical timeline (no early change, then slow improvement). Additionally, it emphasizes the importance of choosing a good clinic: John picked a clinic with a solid reputation, proper licenses, and an orthopedic focus. This gave him confidence in the cell product quality and procedure, which likely contributed to a positive result with no complications.
Every patient is different. Age, severity of condition, overall health, and even genetic factors can influence how well MSC therapy works. But stories like John’s, echoed by many patient testimonials, underscore why people are exploring stem cells in Cancun and Tijuana – it can offer a new lease on life for those who had run out of options.
FAQs (Frequently Asked Questions)
Q: Is stem cell therapy painful?
A: The procedure itself is usually not very painful. Most MSC treatments involve only needle-based procedures. If you are having a bone marrow aspiration for autologous MSCs, you will get local anesthesia – you might feel pressure or brief pain during the draw, but it’s generally well-tolerated (some describe it as uncomfortable but not intolerable). For injections into joints or IV infusions, those feel similar to getting a shot or an IV line; the area may be numbed for joint injections so you might just feel pressure. After the treatment, some pain can emerge at the injection site – for example, joint injections can cause temporary soreness or a mild inflammatory reaction for a few days. Bone marrow draw sites can ache for a couple of days as they heal. Clinics often provide pain medication for aftercare, but many patients find they only need over-the-counter analgesics if anything. In summary, discomfort is typically minimal and short-lived. Patients frequently comment that the procedure was easier than they anticipated. Of course, pain tolerance varies, but serious pain is uncommon. If you’re very anxious about needles or procedures, discuss this with the doctor – mild sedation can be arranged to make you more comfortable.
Q: Is it a cure? Will stem cells completely fix my condition?
A: It’s important to set realistic expectations: MSC therapy is not usually a “cure”, especially for chronic degenerative conditions. Think of it as a cutting-edge treatment that can significantly improve symptoms and potentially slow progression of a disease, but it often won’t erase the condition entirely. For example, if you have bone-on-bone knee arthritis, an MSC injection might reduce your pain and improve mobility (as it did for John in the scenario), but it won’t regenerate a brand-new perfect cartilage layer in most cases. It can delay or avert the need for surgery, but it’s not turning the clock back to youth. In autoimmune diseases like rheumatoid arthritis or multiple sclerosis, MSC therapy can push the disease into remission or reduce flares, but it may not be a permanent cure – the underlying propensity for autoimmunity might still be there, and other therapies might still be needed. That said, there are instances where patients have had near-complete resolution of symptoms for a long period. For instance, some orthopedic patients get years of relief from one injection. But these outcomes aren’t guaranteed for everyone. It’s safest to view MSC therapy as a very promising treatment – one that might significantly improve your quality of life – but not a 100% guaranteed cure-all. Be cautious of anyone advertising it as a “miracle cure.” Science shows improvement (sometimes dramatic), not magic. If it does cure you, fantastic – but go in with hopeful yet measured expectations.
Q: What about long-term safety? Are there risks down the road?
A: Thus far, MSC therapies have shown a very favorable safety profile in clinical studies . Unlike embryonic stem cells, adult MSCs are not known to form tumors or teratomas – they have been used in thousands of patients with no reports of that kind of complication. Short-term, the main risks are minor: possible injection site pain, transient fever or immune reaction (rare), or infection if the injection is not done sterilely (which is exceedingly rare in proper clinics). Long-term, studies with follow-ups of a few years have not found significant late-onset issues. For example, meta-analyses in knee osteoarthritis found no increase in adverse events for MSC-treated patients compared to controls even at 12+ months . Similarly, in autoimmune disease trials, there were no higher rates of infections or malignancies in MSC recipients vs placebo . That said, “long-term” in the context of a relatively new therapy means perhaps 5-10 years of data at most. It’s reassuring that in that timeframe we haven’t seen red flags. There is ongoing monitoring in clinical trials to ensure safety remains high as time goes on. One theoretical concern was whether donor MSCs could be rejected or cause immune reactions – in practice, MSCs are naturally immune-privileged to an extent, and most people tolerate donor cells without problems (some mild reactions like a fever or chill can occur in a small fraction of IV infusions, but these pass quickly). To date, no serious long-term complications (such as increased cancer risk or organ damage) have been attributed to MSC therapy. Leading researchers consider MSC treatments safe enough that they’re being tested in fragile populations (like children with disorders, or patients with severe heart failure, etc.). Of course, as with any medical intervention, unforeseen risks could potentially emerge with larger numbers of patients and longer follow-up, but the data right now is very reassuring. Choosing a licensed, high-quality clinic also mitigates risks (ensuring the product you get is pure and uncontaminated, for example). Always have a thorough discussion with the treating physician about the risk/benefit, but you can take comfort in the fact that safety is one of the strongest aspects of MSC therapy so far.
Q: How do I know if I’m a good candidate for MSC therapy?
A: Determining candidacy is crucial. Generally, you might be a good candidate for MSC therapy if:
· You have a condition that research suggests MSCs can help. This includes moderate osteoarthritis (joints that have some cartilage left to save, rather than fully collapsed joints), certain tendon/ligament injuries, and some chronic inflammatory or autoimmune conditions. If your condition is very end-stage (e.g., a joint that is completely destroyed/bone-on-bone), MSCs might still help pain, but the regenerative potential is lower. In such cases, the doctor might temper expectations or suggest other interventions.
· You’ve tried standard treatments without adequate relief. For instance, for joint pain you may have done physio, medications, maybe steroid or gel injections. Or for autoimmune disease, you’ve tried first-line drugs. MSC therapy often comes into play when conventional options fail or have side effects, and you’re looking for something novel.
· Your overall health is reasonably good. You don’t necessarily have to be super healthy, but certain serious health issues might exclude you – for example, an active infection or a current cancer (oncologists typically advise against stem cell therapies if you have active cancer, because theoretically growth factors could interact with cancer, although MSCs themselves are not known to cause cancer, but it’s cautionary). Uncontrolled diabetes or other conditions might need to be optimized before therapy to improve healing.
· You’re not pregnant or nursing (as a precaution, most clinics won’t treat pregnant women with MSCs because it hasn’t been studied).
· For autologous therapy: you need to have a viable source of cells. Extremely elderly or frail patients might have fewer harvestable MSCs (though even in folks in their 70s, bone marrow and fat still have MSCs, just not as many as younger people). In such cases, clinics often turn to donor cells.
The best way to know is to have your case evaluated by a knowledgeable physician. They might ask for imaging or lab tests depending on the issue. A reputable clinic will tell some people, “Sorry, we don’t think stem cells are appropriate for you.” For example, if someone has complete bone collapse in a joint, they might direct them to a surgical option instead. Or if someone’s condition is too advanced or alternative therapy would be more effective, a good clinic will say so. If you self-assess, look at your condition and see if it matches those discussed in reputable sources. Also, consider your timeline: if you need immediate relief within days (say, for acute severe pain), stem cells won’t act that fast – they are better for longer-term healing. On the other hand, if you have patience and your condition is appropriate, you could be an excellent candidate who stands to gain a lot. Finally, being a “candidate” also means understanding the commitment – you might need to travel, possibly repeat treatment, and follow post-treatment instructions. Ensure you’re up for that. In summary, candidacy comes down to: having a treatable condition, having tried other therapies first, being medically suitable for an injection/infusion, and having realistic expectations. Consult with a trusted medical professional to make the final call.
Closing Summary
In closing, mesenchymal stem cell therapy in Cancun or Tijuana represents a cutting-edge option at the forefront of regenerative medicine. For patients suffering from joint pain, injuries, or certain chronic illnesses, it offers a new avenue when conventional treatments have fallen short. We’ve discussed how MSCs can help conditions like osteoarthritis (by easing pain and possibly slowing joint damage), tendon injuries (by boosting healing), autoimmune diseases (by calming the immune system), and even aiding recovery in neurological injuries. The scientific evidence – especially recent studies from 2023–2025 – provides a growing foundation that this isn’t just hype; there are real, measurable benefits being observed in clinical trials . Moreover, the safety profile of MSC therapy is solid, with low incidence of adverse effects in studies spanning thousands of patients .
Mexico, in particular, has become a leader in offering regenerative therapies, partly due to a supportive regulatory environment that allows advanced techniques (like culturing cells) under proper oversight. Both Cancun stem cell clinics and Tijuana stem cell clinics operate under COFEPRIS regulations, which, as we noted, enforce quality standards akin to international norms. A legitimate clinic will have highly trained physicians and utilize GMP labs, ensuring that patients receive treatments that are safe as well as potentially effective . When done in such a professional setting, MSC therapy is not “experimental” in the wild west sense, but rather an evidence-based, protocol-driven procedure grounded in many years of research.
That said, it’s not a magical panacea. We’ve avoided any salesman language here because, truthfully, stem cell therapy is not about miracles – it’s about scientific progress and giving the body tools to heal itself. Patients considering this route should do so with informed optimism: you have reason to be hopeful, but always have a candid discussion with the treating team about what outcomes are realistic for you. For some, MSC therapy will be life-changing, for others it might be modestly helpful, and a few may not notice much effect – just like any medical treatment.
If you decide to explore MSC therapy in Tijuana or Cancun, use the information in this guide to navigate the journey: pick a reputable clinic, ensure you fit the criteria, and prepare for the process as explained. Many patients report positive experiences, not only with the treatment but with the care and attention they receive from clinics in Mexico (which often pride themselves on patient-centric service). The cost savings compared to the U.S., coupled with the chance to recuperate in a nice locale, are added bonuses – but the real reward is the potential improvement in your health and well-being.
In summary, mesenchymal stem cell therapy has moved from the realm of theory to tangible practice. Whether it’s helping a grandmother avoid a knee replacement or giving an athlete a second chance after injury, the therapy is delivering outcomes that matter. If you’re seriously considering it, arm yourself with knowledge (we hope this article served that purpose), consult with professionals, and weigh the pros and cons. MSC therapy in Cancun or Tijuana is evidence-based, regulated, and worth exploring – provided you do so with trained medical professionals and realistic expectations. It could be the treatment that helps turn your health situation around, or at the very least, a stepping stone towards better management of your condition. Always remember: the goal is to improve your quality of life and functionality safely, and in that regard, MSC therapy is a promising tool on the cutting edge of modern medicine.
Sources:
1. Cao M. et al. (2025). Stem Cell Research & Therapy – Meta-analysis of MSC injections for knee osteoarthritis showed significant 6- and 12-month improvements in pain (WOMAC, VAS) and function, with no increase in adverse events compared to controls .
2. Lee SY. et al. (2021). Annals of Rehabilitation Medicine – Systematic review of tendon injuries found MSC therapy improved pain, function, and even MRI/ultrasound evidence of tendon healing, with a dose-dependent effect on pain relief .
3. Zeng L. et al. (2025). Stem Cell Research & Therapy – Meta-analysis of 42 RCTs in autoimmune diseases (RA, lupus, etc.) concluded MSC transplants improved clinical symptoms in several conditions (like RA and lupus) and did not increase adverse effects, supporting a strong safety profile .
4. Shen Z. et al. (2024). Stem Cells Translational Medicine – Systematic review and meta-analysis in ischemic stroke patients found MSC treatment led to better recovery (improved activities of daily living and neurological scores) and lower mortality versus placebo, with only minor side effects (e.g. transient fever) .
5. Open Access Maced J Med Sci. (2023). – Comparative study indicating MSC therapy has superior outcomes in knee osteoarthritis compared to PRP, and that adding PRP to MSC provides no significant additional benefit over MSCs alone .
6. Reddit - r/stemcells (2022). – User-posted comprehensive checklist highlighting COFEPRIS licensing requirements for Mexico clinics (collection license, lab license, regenerative medicine license) and advising patients to verify a clinic’s licenses and credentials for safety .
7. Biomedcentral – Review on MSCs (2024) – General background on MSC biology: MSCs are multipotent, can self-renew and differentiate, and have immunomodulatory and anti-inflammatory properties, making them valuable in regenerative therapies .

Comments